The 4 Most Common Types of Arthritis – And the 4 Stages of How It Progresses

Doctor, is arthritis the same for everyone?
This is one of the most frequent questions I get from my patients — and the answer is no. Arthritis is not a single disease. It has multiple types, causes, and progression patterns.
While all forms of arthritis affect the joints, they differ in how they develop, what causes them, and how they impact your mobility and comfort. Understanding these differences helps in choosing the right treatment at the right time.
In this blog, I’ll walk you through the four most common types of arthritis I see in my clinic — and explain the four stages through which arthritis usually progresses if left untreated.
The 4 Most Common Types of Arthritis
1. Osteoarthritis (OA) – The Wear-and-Tear Arthritis
Osteoarthritis is the most common form of arthritis, often linked with ageing.
- It occurs when the protective cartilage that cushions the ends of bones wears down over time.
- Common in the knees, hips, hands, and spine.
- Symptoms: pain during movement, stiffness after rest, swelling, and a grinding or clicking sound.
- Risk Factors: age, obesity, repetitive strain, and old injuries.
This is the form of arthritis I see most often — especially in patients above 50 who have gradually lost mobility in their knees or hips.
2. Rheumatoid Arthritis (RA) – The Autoimmune Type
Unlike osteoarthritis, RA is an autoimmune disorder — meaning the body’s immune system mistakenly attacks its own joints.
- It causes chronic inflammation in the lining of the joints (synovium).
- Often affects smaller joints like fingers and wrists first, then spreads to larger ones.
- Symptoms: swelling, pain, fatigue, and stiffness, especially in the morning.
- It can also affect the heart, lungs, and eyes if left uncontrolled.
Early diagnosis and medication are crucial to prevent permanent joint damage in RA.
3. Post-Traumatic Arthritis – The Result of Injury
This form of arthritis develops after a significant joint injury — like a fracture, ligament tear, or sports trauma.
- Damage from the initial injury disrupts the smooth cartilage surface, leading to early wear and tear.
- Common in younger patients or athletes.
- Symptoms: pain that appears months or years after the injury, stiffness, and reduced joint function.
Many of my sports patients develop post-traumatic arthritis years after an ACL or meniscus injury. Early management prevents it from worsening.
4. Gout – The Metabolic Arthritis
Gout is caused by excess uric acid crystals depositing in the joints, usually the big toe, ankle, or knee.
- Symptoms: sudden, intense pain, redness, and swelling.
- Often triggered by high-purine foods, dehydration, or alcohol consumption.
- Common in men over 40.
Gout is extremely painful but highly manageable with dietary control and medication.
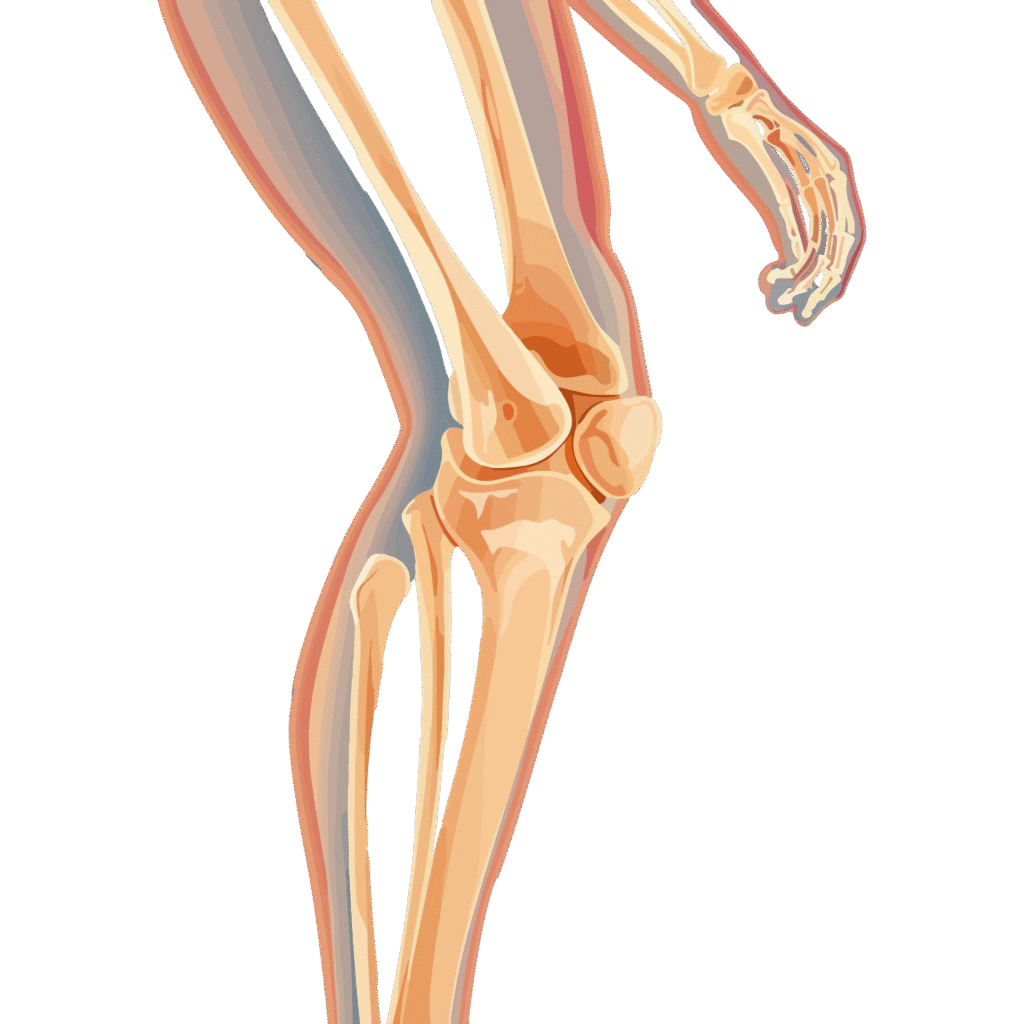
The 4 Stages of Arthritis Progression
Regardless of the type, arthritis tends to follow a predictable pattern as it worsens. Recognising which stage you’re in can guide your treatment decisions.
Stage 1: Minor (Early Stage)
- Mild discomfort or stiffness after activity.
- No visible changes on X-rays.
- Preventive care and lifestyle changes can stop it here.

Stage 2: Mild (Cartilage Weakening)
- Noticeable joint stiffness and occasional pain.
- X-rays show narrowing of joint space.
- Conservative treatment — physiotherapy, weight control, and medications — is effective.
Stage 3: Moderate (Cartilage Loss)
- Frequent pain even at rest.
- Bone spurs start forming as the body tries to protect the joint.
- Limited range of motion and swelling.
- Intra-articular injections or minimally invasive procedures may help.
Stage 4: Severe (Advanced Stage)
- Complete loss of cartilage, bones rubbing directly against each other.
- Constant pain, deformity, and reduced mobility.
- At this stage, joint replacement surgery becomes the best solution for regaining mobility and comfort.
Why Understanding the Type and Stage Matters
Each patient’s arthritis journey is unique. A young athlete with post-traumatic arthritis needs a very different approach than a senior citizen with osteoarthritis.
Knowing your type and stage allows your doctor to personalise treatment — whether it’s medications, physiotherapy, regenerative techniques like PRP, or advanced robotic joint replacement for end-stage cases.
Final Thoughts
Arthritis doesn’t happen overnight, and it doesn’t have to take away your quality of life. The key lies in early diagnosis, correct classification, and proactive management.
If you’re struggling with joint pain, don’t wait for it to become severe. Get evaluated, understand which type you have, and start treatment early.
As I often tell my patients:
“The earlier we act, the longer your joints last.”